RE: [Critical Care Nutrition] Digest for criticalcarenutrition@googlegroups.com - 2 updates in 1 topic
MacEachern, Judy
Hi Meg,
We had a good discussion about this with a group of ICU RDs at a recent event. Some good points brought up:
1) Few RDs (no one in our group of at least 15 ICU RDs) has the time to calculate NUTRIC on every patient. I tried calculating on a few in the past. APACHE II is something like 12 (?) items and SOFA is 7. After scoring a few patients, you can start to see how patient presentation may pan out (e.g., a young person with no previous co-morbidities presenting acutely with ALI and only one organ involvement is likely to score low).
2) Nutrition risk is not the same as nutrition status. A malnourished patient could potentially score low on NUTRIC. Would we not feed that patient?
3) For all the effort RDs have done to start some tube feed (i.e., “just get something going”), it seems difficult to now come into the ICU and say “feed this one”, “feed that one”, etc. (Especially when trying to disseminate current evidence to such a large group of nurses, allied health, intensivists.)
4) If a feed starts on the weekend with no RD present, and we evaluate NUTRIC as low – what then?
5) What happens to the patient that deteriorates in the ICU? The APACHE II is about presentation in the first 24 h of ICU admission. Much can change in the following days.
It’s difficult to know when to feed patients. Especially when studies came out that didn’t show positive changes in clinical outcomes. However, a good portion of those studies excluded malnourished patients.
At the end of our discussion, most RDs felt it is good that risk assessment tools are being developed, but few RDs were going to significantly change their practice based on the existing tools.
Hope this helps. Best regards,
Judy
Judy MacEachern RD CDE
Clinical Dietitian
ICU, Surgery, Paediatrics, Paediatric Diabetes Program
Guelph General Hospital
Telephone: 519-837-6440 ext.2822
Pager: 519-244-0362
From: criticalca...@googlegroups.com [mailto:criticalca...@googlegroups.com]
Sent: April-20-16 1:08 AM
To: Digest recipients
Subject: [Critical Care Nutrition] Digest for criticalca...@googlegroups.com - 2 updates in 1 topic
· NUTRIC score usage - 2 Updates
|
megan.n...@gmail.com: Apr 19 10:27AM -0700
|
|
michael wintering <michael....@gmail.com>: Apr 19 12:18PM -0600
|
|
You received this digest because you're subscribed to updates for this group. You can change your settings on the
group membership page. |
--------------------------------------------------------------------------------
CONFIDENTIALITY NOTICE: This message, including any attachments, is intended only for the use of the intended recipient(s) and may contain information that is privileged, confidential and prohibited from unauthorized disclosure under applicable law. This material may be subject to the provisions of the Freedom of Information and Protection of Privacy Act or the Personal Health Information Protection Act. If you are not the intended recipient or have received this message in error, please notify us immediately by reply e-mail and permanently delete original transmission. Thank you.
Daren Heyland
Hi all
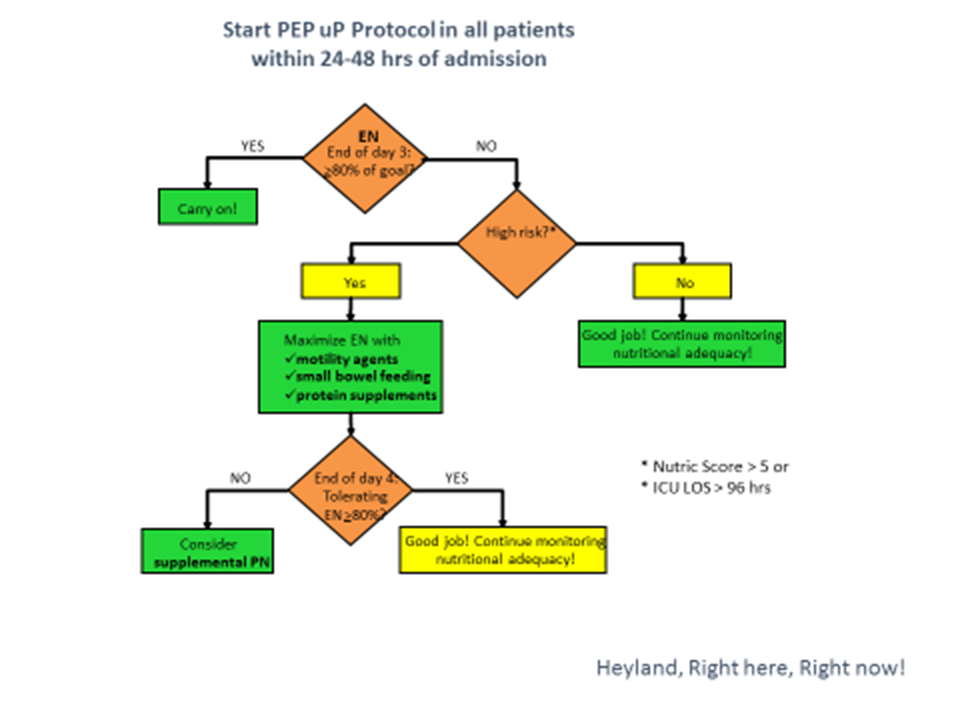
Thanks for your interest in the NUTRIC score. I would like to clarify somethings that may help with the uptake of the NUTRIC score. The NUTRIC score was not intended to be done on all patients on day 1 or day 2 as a way of determining whether to start feeds or not; but rather, as a tool to help you determine whether maximizing effort to maximize intake will really matter. As indicated in the figure below, I recommend using NUTRIC on day 3 (or so) when you are asking the question, “Is this patient receiving at least 80% of what you are prescribing them”. If that answer to that question is ‘no’, then knowing the NUTRIC score will help you allocate your time and energy in those patients that matter the most. It is a true that a patient on day 3 that has a low NUTRIC score may evolve into a high risk patients (particularly if their stay becomes prolong) so you need to keep watching them but efforts to maxming delivery can be postponed till you are sure they are high risk. I agree with Judy that nutrition risk is not the same as nutrition status and that you still need to be considerate of whether the patient is malnourished or not in making your decision about whether to maximize intake. So in essence, there are 4 risk groups in order of highest risk to lowest risk:
High nutric and malnourished
High nutric and not malnourished
Low nutric but malnourished
Low nutric and not malnourished
The key point is that not all patients will benefit the same from our efforts to feed them. We need to re double our efforts to see that higher risk patients reach that 80% level, for them to achieve optimal outcomes (observational level of evidence). The reason the RCTs don’t confirm this benefit is because they enroll all 4 of those groups, the majority being in the low risk group.
Note, that there is a ‘bedside monitoring tool’ on our website that enables the calculation of the NUTRIC score (you still have to input the variables but it doesn’t the calculation for you and may be more efficient) but don’t use it in everyone and don’t use it at the beginning as a decision who to start. Start nutrition in everyone who is mechanically ventilated and expected to stay a few days and then assess whether achieving near goal is imiportant in these patients on day 3 ish.
Hope that helps,
Daren
--
You received this message because you are subscribed to the Google Groups "Critical Care Nutrition" group.
To unsubscribe from this group and stop receiving emails from it, send an email to
criticalcarenutr...@googlegroups.com.
To post to this group, send email to
criticalca...@googlegroups.com.
Visit this group at
https://groups.google.com/group/criticalcarenutrition.
For more options, visit https://groups.google.com/d/optout.
